ANTIBIOTICS & EUROPE
Or: How I Learned to Stop Worrying and Love the Plague
Antibiotic medications have been a revolutionary weapon in the ongoing fight against disease. Nearly a century ago, microbiologist Alexander Fleming accidentally discovered that certain strains of fungi naturally inhibited the growth of encroaching bacterial colonies. Fleming and his colleagues successfully isolated the compound responsible for bacterial inhibition, called penicillin, the first true antibiotic agent. This would soon become one of the most important inventions of the twentieth century - antibiotic medication. Fleming received the Nobel Prize in Physiology and Medicine in 1945 for his work.
It is unclear just how many lives would be saved as a result of this brilliant accident, perhaps too many to count. In 1900, the three leading causes of death were pneumonia, tuberculosis, and gastroenteritis - each of which stem from bacterial infection. In 1997, the three leading causes of death were heart disease, cancer, and stroke (CDC). Antibiotics changed the game for medicine in the twentieth century.
Today, antibiotic medications continue to play a vital role in combating a variety of diseases. However, a growing threat appears to be looming over the horizon, a threat that Fleming himself predicted, as he wrote in his personal journal:
"The thoughtless person playing with penicillin treatment is morally responsible for the death of the man who succumbs to infection with the penicillin-resistant organism."
As it turns out, Fleming was right to be concerned about the inevitable backlash of microbial resistance. The act of using antibiotics kills off susceptible bacteria, and at the same time inadvertently selects for organisms that are immune to its effects. Over time, these genetic adaptations proliferate throughout bacterial populations. If given enough time, the same bacterial threats that plagued the world a century ago could overcome all known antibiotic medications, setting the medical field back nearly a hundred years. The effects of such a setback could be catastrophic. The problem has become so widespread that the World Health Organization has listed microbial resistance as one of the top ten threats to global health in 2019 (WHO).
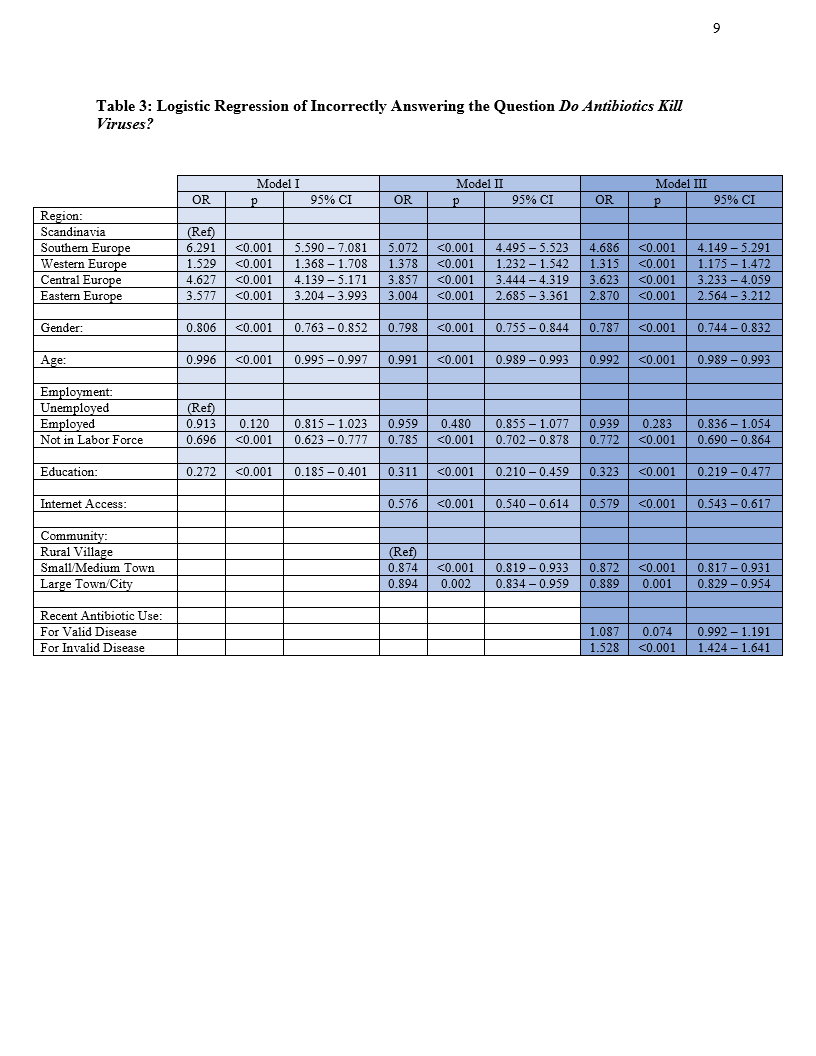
Therefore, it is essential that the general public is aware of how to properly handle antibiotic prescriptions, such as only taking antibiotics for bacterial infections, or continuing to follow through with a prescription even after symptomatic effects disappear. A colleague and I took great interest in this ongoing problem, and came across a set of data surveying more than 25,000 participants from 29 European countries that inquired about general knowledge of how to properly handle antibiotics. Our paper on this subject is included below. Ultimately, we determined that there are specific regions of Europe that score quite low on knowledge about proper antibiotic protocol (specifically Southern Europe), while other regions seem to have a fair understanding (particularly Scandinavia). After adjusting for potential confounding factors, such as demographics, education, occupation, internet access, and more, we were unable to accurately determine what is causing this discrepancy in understanding across regions. We feel that further investigation is warranted to improve public perception about this problem.